|
Guanine's Multi-analyte Multi-omics Sensor
Guanine's sensor quantifies low concentrations by binding targets to microparticles conjugated with millions of electroactive polyGuanine oligonucleotides. This avoids resource-intensive PCR or time-intensive cultures. Microparticle-target-electrode sandwiches are formed on the sensor and an inexpensive potentiostat produces electrical current peaks proportional to each target’s concentration. |
|
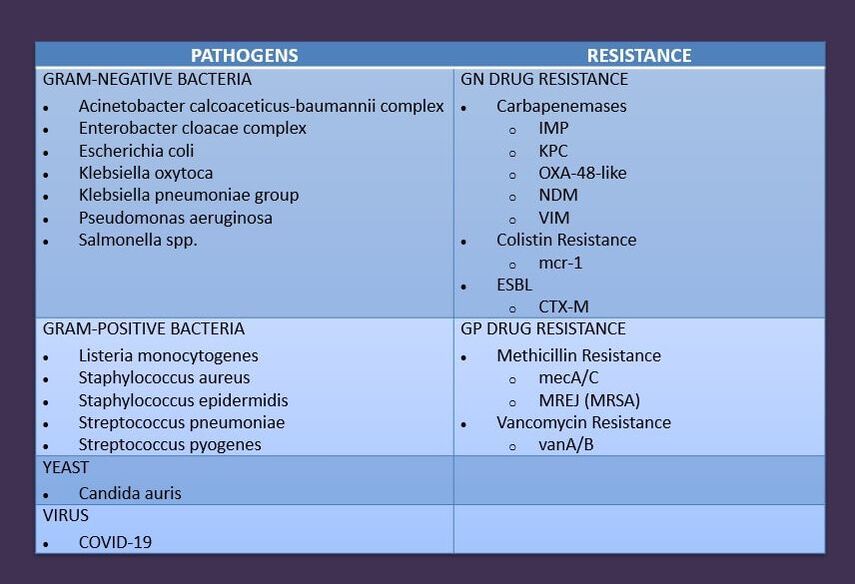
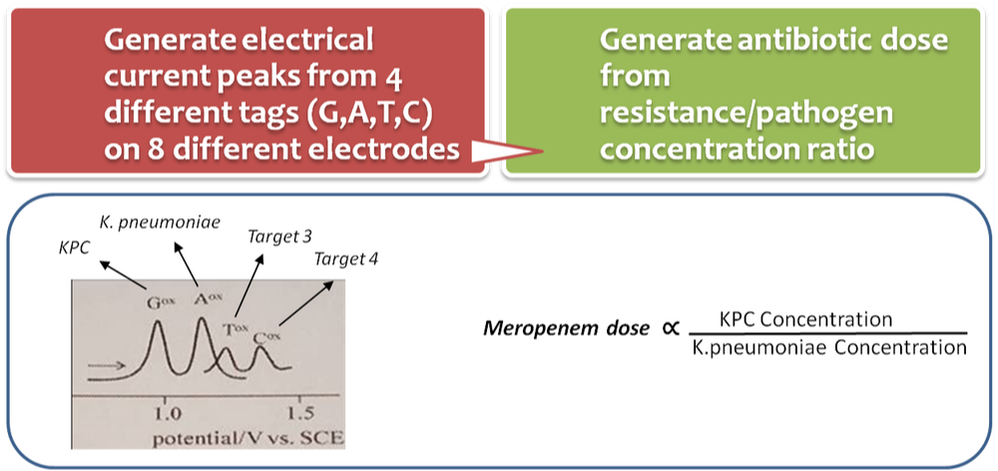
Guanine’s 1 hour quantitative test will detect and quantify 32 sepsis-causing pathogens and drug resistance biomarkers in a single sample with Guanine's mobile reader. A sandwich hybridization assay binds RNA lysed from microbial cells to microparticles conjugated with millions of electrochemically detectable oligonucleotide tags (EC-DOTs) and a carbon working electrode. Multiple electrodes and different microparticle conjugates enable high multiplexing from a single sample. Test software converts oxidation signals to target concentrations using pre-determined formulas. Antibiotic dose is generated from the resistance/pathogen concentration ratio which is pre-calibrated.
|
|
Guanine's Mobile Reader
Guanine's mobile reader operates Guanine syndromic test cartridges and requires no user involvement or lab. Its small size is ideal for testing at the patient’s site. Features include:
|
|
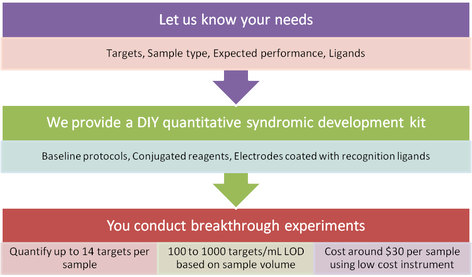
Guanine’s DIY Syndromic Microtiter Kit is a multiplex sandwich assay built on electrochemical sensor electrodes. The kit contains a 96 well sensor microtiter that can quantify up to 14 low concentration nucleic acid targets and/or protein targets in duplicate wells.
|
Principles Of The Assay
|
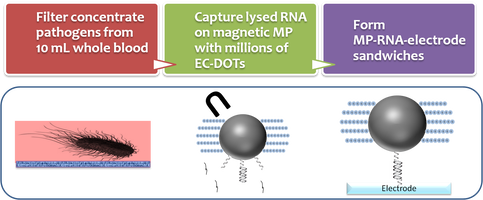
Sample preparation
A liguid or liquefied sample is filtered to concentrate analytes captured on the filter. Large sample volumes are preferred to increase the quantity of analytes. The filter retentate is lysed and mixed with magnetic microparticles that are pre-conjugated with highly specific ligands and millions of electrochemically detectable oligonucleotide tags (EC-DOTs). The solutions are then placed in a magnetic capture microtiter unit to separate magnetic microparticle-target complexes from nonspecific materials. After a wash, the resuspended solutions are transferred to sensor microwells to form microparticle-target-electrode sandwiches. |
|
|
Detection and quantification
A differential pulse voltammetry scan generates a peak oxidation signal for each sandwich group which corresponds to the concentration of the associated target in the sample. The test results are transmitted to a smart phone app which converts the signals from each sandwich group into a concentration level using a pre-calibrated concentration curve adjusted by the test controls. Each sensor can produce 4 signal peaks associated with EC-DOTs employing electroactive G, A, T or C detection sequences. Duplicate samples allow 16 unique signal peaks in two microwells for 14 unique targets plus positive and negative controls. |
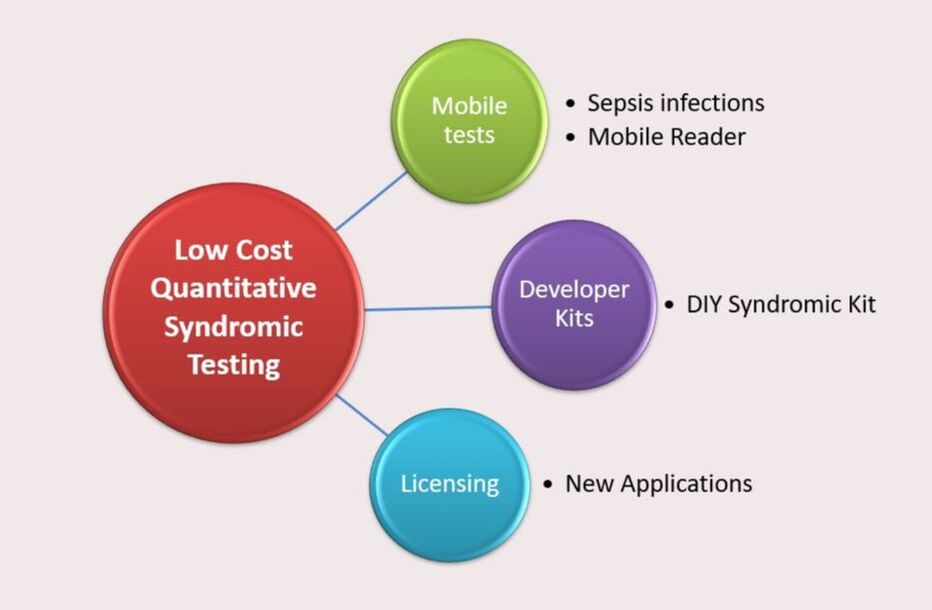
Guanine licensing opportunities include:
- Medical Infections (Blood, respiratory, GI, ticks)
- Biomarkers (Cancer, neurological, cardiac)
- Companion Dx (Efficacy, risk, dose)
- AI/ML (Precision medicine, chronic therapies)
- Industrial Pathogens (Food, water, bioreactors, animals)
- Bioterrorism (Air, insects, people)
* Specifications are subject to change